Introduction
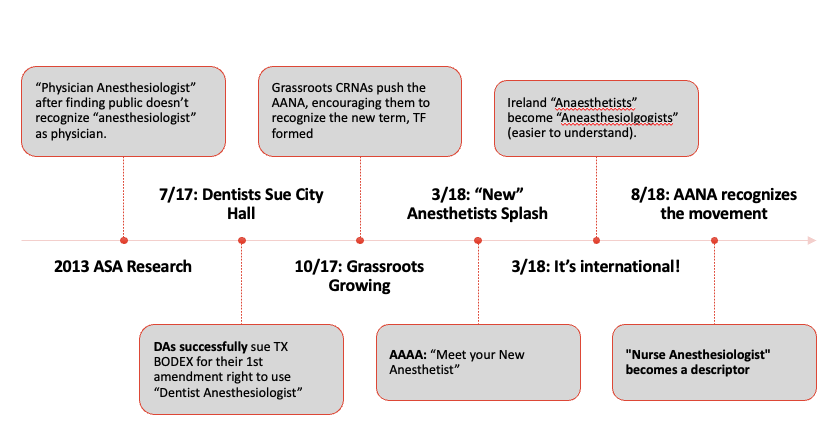
CRNAs have been administering anesthesia since the civil war, and yet confusion still exists regarding the CRNA role. That problem has inspired a network of CRNAs to organize into the Committee for Proper Recognition of CRNAs with the aim of increasing awareness for stakeholders that CRNAs are 1) Advanced Practice Registered Nurses who are 2) experts in anesthesia care. One part of that plan is to begin promoting the term “nurse anesthesiologist” since it more readily communicates the scope of services of CRNAs. Eventually, this resulted in the recognition of the term as an accepted descriptor or even title with certain regulatory bodies, within the association itself, and the updating of the name of the association to the “American Association of Nurse Anesthesiology.”
“With calm, rational education, we’ve seen the initial emotional reaction from physician groups be toned down, and both groups realize it’s possible to recognize the expertise of both physicians and CRNAs and to work together towards mutual goals. ”
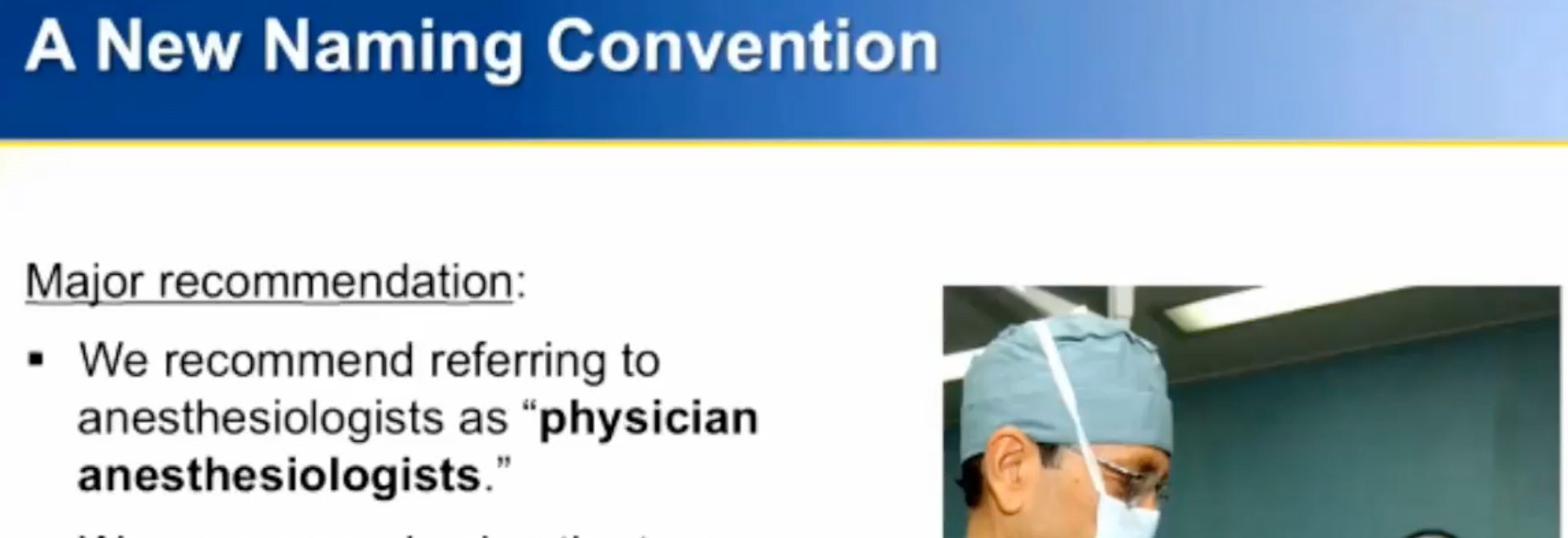
Research Demonstrates Public Doesn’t Equate “anesthesiologist” with “physician” or “doctor”.
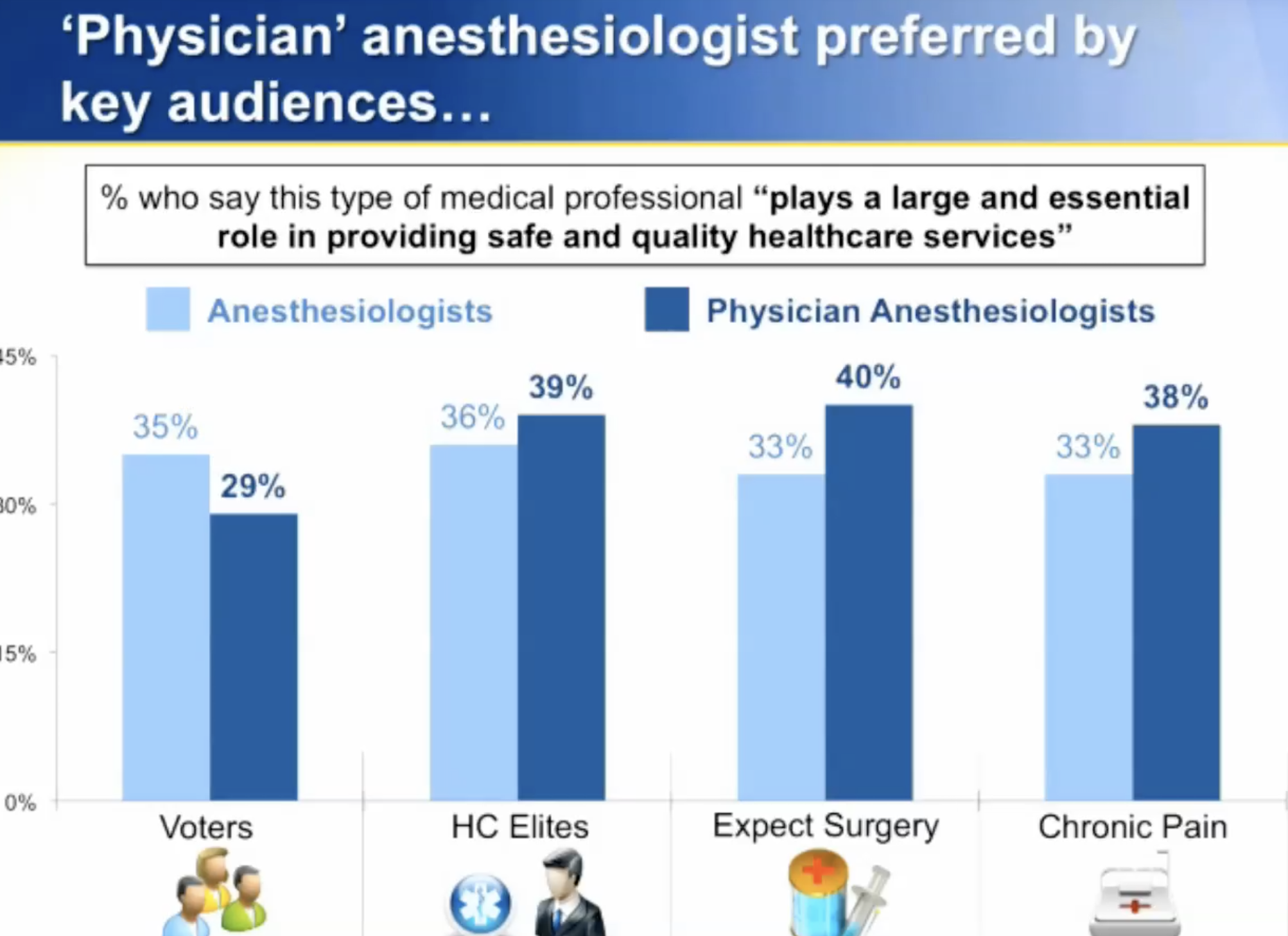
Over the past several years, the American Society of Anesthesiologists (ASA) has begun using the descriptor “physician anesthesiologist”. While not the intent, the usage of the term infers there are other types of anesthesiologists, and that “anesthesiologist” is a neutral term.
Their decision came after they commissioned public relations firms to promote the role of the physician in anesthesiology care.
Below are excerpts from that research, and a photo of the ASA’s publication relations website “When Seconds Count”.
American Academy of Anesthesiologist Assistants (AAAA) usage of “anesthetist”; ASA defines “anesthetist” to include AAs.
Since each of the three independent professions have protected legal titles (physician, dentist, nurse), additional descriptors such as “anesthesiologist” are not protected, especially when paired with the profession that is administering it. Accordingly, when a anesthesia assistant (an assistant who can only administer anesthesia under the supervision of a physician anesthesiologist) administers anesthesia they may legally use the descriptor “anesthetist”. The AAAA/ASA utilized this term in recent publications, demonstrating the descriptive value of terms such as “anesthesiologist” or “anesthetist”.
Further, the ASA also updated their statement on the term “anesthetist”:
Statement on the Anesthesia Care Team
(Approved by the ASA House of Delegates on October 26, 1982 and last amended on October 17, 2018)
Definitions
b. Non-physicians
ANESTHETIST: A nurse anesthetist or anesthesiologist assistant…
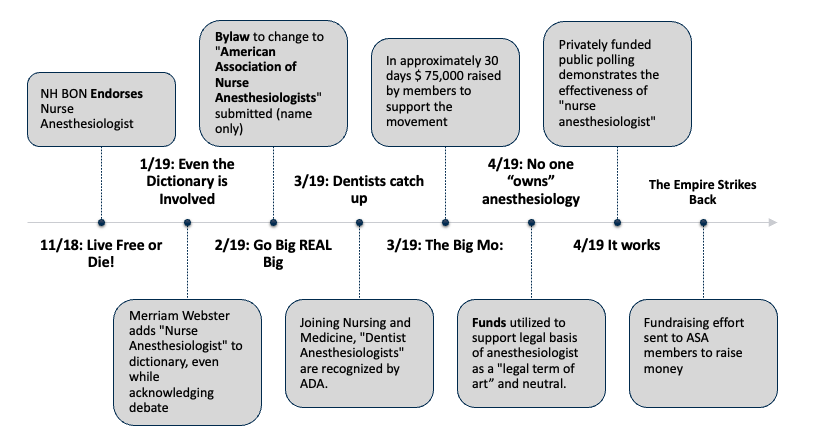
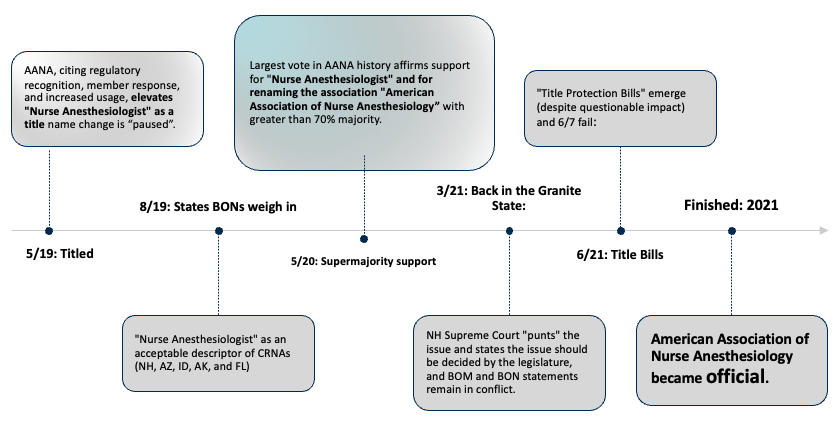
A timeline of events
Public Polling
Ascend Public Polling was commissioned for the survey.
A survey was conducted by on March 28 - April 1, 2019, 4,028 survey respondents were randomly selected from a demographically proportionate sample of registered voters in the United States.
When asked:
“Which term do you feel best describes a professional nurse who provides anesthesia during surgery, a Nurse Anesthetist or a Nurse Anesthesiologist?”
The majority chose Nurse Anesthesiologist (54%) over Nurse Anesthetist (23%).
When asked:
“Which medical professional do you consider to be the expert in the field of anesthesiology, a Nurse Anesthetist or a Nurse Anesthesiologist?”
The gap widens, with the overwhelming majority of respondents, again, choosing Nurse Anesthesiologists (57%) over Nurse Anesthetists (16%).
When asked:
Would you say you recognize a Nurse Anesthesiologist as a member of the nursing profession and a Physician Anesthesiologist as a medical doctor?
By a 3:1 Margin (58% to 18%) respondents stated they recognized the difference between the two professions.
A New Dictionary Entry
In 2019, Merriam Webster Dictionary added a new term to their dictionary, noting that while nurse anesthetist remains more common, nurse anesthesiologist is an established synonym.
nurse anesthesiologist
noun
plural nurse anesthesiologists
Definition of nurse anesthesiologist
: a registered nurse certified to administer anesthetics
Professional Context For Change
In American society, many professions utilize the suffix “ologist” to denote experts in a field of study. Audiologist, epidemiologist, histologist – the list is enormous (greater than 600) and not exclusive to physicians. CRNAs are educated to be and practice as experts in the field of anesthesiology; therefore, the term “nurse anesthesiologist” is consistent, clarifying, and appropriate to describe a CRNA.
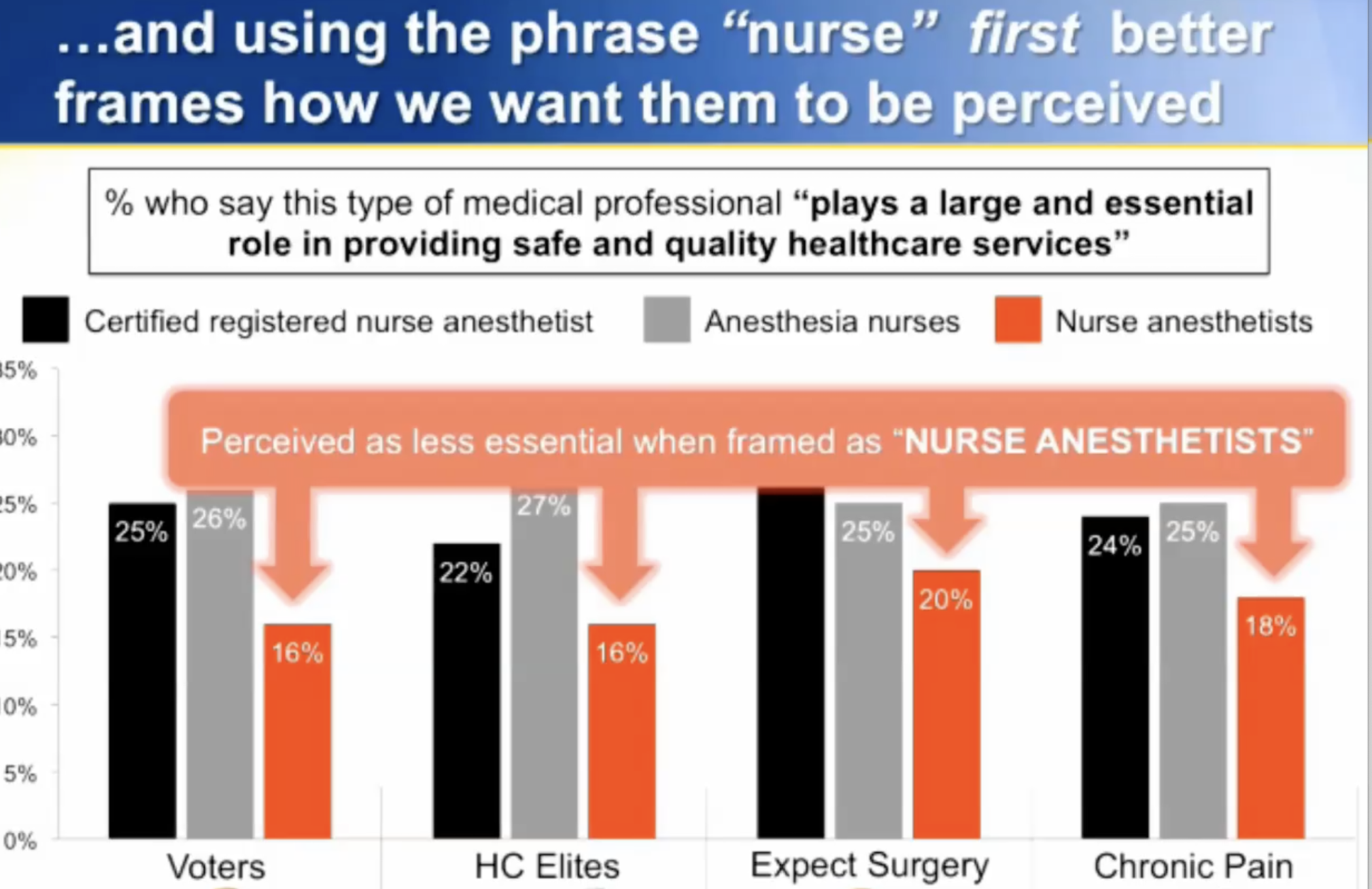
THE ASA. In recent years, the ASA has utilized and promoted the term “Physician Anesthesiologist.” It logically follows that there are other types of anesthesiologists, including “Nurse Anesthesiologists.” Although “physician anesthesiologist” is yet another attempt to raise physician anesthesia providers above nurse anesthetists professionally, their term is accurate. Additionally, ASA messaging research from 2013 has encouraged ASA members to refer to CRNAs simply as “nurses” or “anesthesia nurses.” The public associates these titles with less confidence regarding handling anesthesia and emergencies. Although these titles may be technically accurate, they do not capture the services or expertise that CRNAs offer.
DENTIST ANESTHESIOLOGISTS. “Dentist anesthesiologists” have also gained name recognition in recent years, with their own society and training programs in university settings. To describe CRNAs as “nurse anesthesiologists” accurately portrays that the anesthesia a CRNA provides is of the same class and quality, and no different than that provided by these other types of “anesthesiologists.” See more: asdahq.org
GLOBAL CONTEXT. Citing some of the same concerns as American nurse anesthetists and aligning with global norms, Ireland’s anaesthetists have changed to “anaesthesiologists” and Australia is considering the change as well. See more: “Terminology of ‘anaesthesia’ changed in line with global best practice” and “What’s in a Name?”
DOCTORATES FOR CRNAS. Mandatory doctoral degrees for entry into practice by 2025 further strengthens the argument for using the title "nurse anesthesiologist.” Currently, CRNAs practice as experts in their field, often functioning as independent providers. The mandate that all new providers graduate with a doctoral degree by 2025 demonstrates the profession’s commitment to expertise and independence, further strengthening the argument for the title “nurse anesthesiologist.”
THE AA. Anesthesiologist Assistants (AAs) utilize the term “anesthetist,” adding confusion to the alleged equality of the CRNA and the AA. AAs are often described as anesthetists. AAs have different, shorter training and required clinical experience, and therefore by design and federal law cannot function as independent providers. To use the term “anesthetist” to describe a CRNA while not simultaneously utilizing “anesthesiologist” may inappropriately indicate equality between the CRNA and AA, and inferiority of the CRNA compared to the physician anesthesiologist. Use of the term “nurse anesthesiologist” is clarifying and helps to remove this confusion. See more: anesthetist.org
Legal Opinon
The CPRC commissioned a legal opinion by a respected Chicago law firm to analyze the legal basis of any potential lawsuit regarding changing the name of the AANA to the “American Association of Nurse Anesthesiologists"
“Based on the foregoing, we do not think a legal challenge to the proposed name change particularly one that is founded on a theory that the term “nurse anesthesiologist” is unlawfully misleading or deceptive – would be successful.”
The entire legal opinion is accessible here. and the supplemental analysis of Florida and Texas are accessible here.
“Nurse Anesthesiologist” is Commercial Free Speech
The 5th U.S. Circuit Court of Appeals affirmed June 19 an opinion by a federal district court in Texas, saying certain types of advertising restrictions enforced by the Texas State Board of Dental Examiners on dentists - including dentist anesthesiologists - violated dentists' First Amendment rights to engage in commercial speech.
Notably, the court noted that in order for commercial speech to be protected under the First Amendment, it "must concern lawful activity and not be misleading."
While involving the profession of dentistry and as such having a number of nuances, the parallels are clear: CRNAs who advertise as “nurse anesthesiologists” - itself a term recognized by the national body - are advertising in a way that is “lawful and not misleading” and as such would fall under commercial free speech protection.
Read the entire brief:
http://www.ca5.uscourts.gov/opinions/pub/16/16-50157-CV0.pdf
Anesthesiologist Cannot Be Trademarked
From John M. Wilke, Examining Attorney for the U.S. Patent and Trademark Office (USPTO), the federal agency for granting U.S. patents and registering trademarks
The following supports the argument that “anesthesiologist” is descriptive and not beholden to the medical, nursing, or dental professions.
Merely Descriptive Refusal
Registration is refused because the applied-for mark merely describes the provider of applicant’s services. Trademark Act Section 2(e)(1), 15 U.S.C. §1052(e)(1); see TMEP §§1209.01(b), 1209.03 et seq
A mark is merely descriptive if it describes an ingredient, quality, characteristic, function, feature, purpose, or use of an applicant’s goods. TMEP §1209.01(b); see, e.g., DuoProSS Meditech Corp. v. Inviro Med. Devices, Ltd., 695 F.3d 1247, 1251, 103 USPQ2d 1753, 1755 (Fed. Cir. 2012) (quoting In re Oppedahl & Larson LLP, 373 F.3d 1171, 1173, 71 USPQ2d 1370, 1371 (Fed. Cir.
2004)); In re Steelbuilding.com, 415 F.3d 1293, 1297, 75 USPQ2d 1420, 1421 (Fed. Cir. 2005) (citing Estate of P.D. Beckwith, Inc.
v. Comm’r of Patents, 252 U.S. 538, 543 (1920)).
“A mark may be merely descriptive even if it does not describe the ‘full scope and extent’ of the applicant’s goods or services.” In re Oppedahl & Larson LLP, 373 F.3d 1171, 1173, 71 USPQ2d 1370, 1371 (Fed. Cir. 2004) (citing In re Dial-A-Mattress Operating
Corp., 240 F.3d 1341, 1346, 57 USPQ2d 1807, 1812 (Fed. Cir. 2001)); TMEP §1209.01(b). It is enough if a mark describes only one
significant function, attribute, or property. In re The Chamber of Commerce of the U.S., 675 F.3d 1297, 1300, 102 USPQ2d 1217, 1219 (Fed. Cir. 2012); TMEP §1209.01(b); see In re Oppedahl & Larson LLP, 373 F.3d at 1173, 71 USPQ2d at 1371.
Applicant has applied for registration of the term NURSE ANESTHESIOLOGIST for “Medical services, namely, anesthesia” in Class
44. Applicant’s proposed mark is merely a combination of merely descriptive terms. The term “NURSE” is defined as “A person trained to care for the sick or infirm, especially in a hospital.” (See attached definition found
at https://en.oxforddictionaries.com/definition/us/nurse ). The term ANESTHESIOLOGIST is defined as “A physician specializing in anesthesiology.” (See attached definition found
at: https://www.ahdictionary.com/word/search.html?q=anesthesiologist). The term ANESTHESIOLOGY is defined as “The branch of medicine concerned with anesthesia and anesthetics.” (See attached definition found on the Internet
at: https://en.oxforddictionaries.com/definition/us/anesthesiology#anesthesiology ). Taken together, the term NURSE ANESTHESIOLOGIST merely describes a nurse trained in providing anesthesia services
Generally, if the individual components of a mark retain their descriptive meaning in relation to the goods and/or services, the combination results in a composite mark that is itself descriptive and not registrable. In re Fat Boys Water Sports LLC, 118 USPQ2d 1511, 1516 (TTAB 2016) (citing In re Tower Tech, Inc., 64 USPQ2d 1314, 1317-18 (TTAB (2002)); TMEP §1209.03(d); see,
e.g., Apollo Med. Extrusion Techs., Inc. v. Med. Extrusion Techs., Inc., 123 USPQ2d 1844, 1851 (TTAB 2017) (holding MEDICAL EXTRUSION TECHNOLOGIES merely descriptive of medical extrusion goods produced by employing medical extrusion technologies.) In the present case, both terms retain their descriptive meaning in connection with the services.
“As noted in the attached evidence and previously cited definitions, an “anesthesiologist” is ordinarily a physician and an “anesthetist” is ordinarily a nurse. However, since anesthesiologists and anesthetist both provide anesthesia services, this distinction does not diminish the descriptive or generic meaning of the term NURSE ANESTHESIOLOGIST used in connection with medical personnel providing anesthesia services, regardless of whether they are nurses or physicians.”
Terms that describe the provider of a product or service may also be merely descriptive of the product and/or service. See In re The Chamber of Commerce of the U.S., 675 F.3d 1297, 1301, 102 USPQ2d 1217, 1220 (Fed. Cir. 2012) (affirming Board’s finding that NATIONAL CHAMBER was merely descriptive of online service providing directory information for local and state chambers of commerce and business and regulatory data analysis services to promote the interest of businessmen and businesswomen); In re Major League Umpires, 60 USPQ2d 1059, 1060 (TTAB 2001) (holding MAJOR LEAGUE UMPIRE merely descriptive of clothing, face masks, chest protectors and shin guards); TMEP §1209.03(q). Attached is evidence found on the Internet of descriptive uses of the terms “anesthesiologist” and “nurse anesthestist” in connection with providers of anesthesia services. See:
https://en.wikipedia.org/wiki/Anesthesiologist https://www.allnursingschools.com/articles/become-nurse-anesthetist/ https://www.google.com/?gws_rd=ssl
As noted in the attached evidence and previously cited definitions, an “anesthesiologist” is ordinarily a physician and an “anesthetist” is ordinarily a nurse. However, since anesthesiologists and anesthetist both provide anesthesia services, this distinction does not diminish the descriptive or generic meaning of the term NURSE ANESTHESIOLOGIST used in connection with medical personnel providing anesthesia services, regardless of whether they are nurses or physicians.
Accordingly, since the proposed mark merely describes the provider of applicant’s services, registration must be refused under Trademark Act Section 2(e)(1), 15 U.S.C. §1052(e)(1); see TMEP §§1209.01(b), 1209.03 et seq.
Arguments for Certified Registered Nurse Anesthesiologist
“Nurse Anesthesiologist,” , on its own, is self-evident. Notably, AANA bylaws specifically reference anesthesiology. This section will review the arguments for acknowledging “Nurse Anesthesiologist.”
Special thanks to Gregory Y. Harris, JD, for his significant contributions to the following two sections. Mr. Harris has been recognized as his peers as a respected national voice on administrative, regulatory and healthcare law and was the recipient of the 2018 Distinguished Achievement Award from the National Council of State Boards of Nursing.
Description of work of a CRNA - are CRNAs practicing anesthesia or anesthesiology?
The first question is whether the “nurse anesthesiologist” accurately describes the legal scope of practice a CRNA may perform. The resolution of this question would be governed by the scope of practice in each state. If a CRNA has the legal authority to make clinical decisions about the delivery of services that include anesthesiology (i.e., the determination of dosing and administration of anesthetics and delivery of anesthesia services), then the use of the term would meet the objective of describing the work to be done – and which is capable of being done – by the CRNA.
Nurse Anesthesiologist is not misleading as it uses the word “nurse” in the title.
On its face, “nurse anesthesiologist” truthfully reports that the person using the title is a nurse. This modifier should be sufficient to satisfy concerns that the use of the term might be creating the false impression that user is a medical doctor.
Likewise, assuming a CRNA has the legal authority to make clinical decisions about the delivery of services that include anesthesiology (i.e., the determination of dosing and administration of anesthetics and delivery of anesthesia services), then the use of the term “nurse anesthesiologist” would truthfully convey accurate information that the user is legally permitted to perform those services.
Nurse Anesthesiologist is protective in states with laws prohibiting representing oneself as a physician.
Commonly, nurse anesthetists are confused for physicians because the scope of their services overlaps both medicine and dentistry significantly. Numerous CRNAs have reported this phenomenon; some CRNAs simply state they are “with anesthesia.” This ambiguity could reasonably lead a patient to conclude that a nurse anesthetist is a physician, and nurse anesthetists who do not clarify may be in violation of the law. As such, “nurse anesthesiologist” can afford these members legal protection by distinguishing themselves as nursing professionals rather than medical doctors.
Public perception research indicates “anesthesiologist” is merely descriptive and not assigned to a single profession
Research from the ASA indicates that the majority (55%) of the country does not recognize an “anesthesiologist” as a physician. They are correct since both nurses and physicians can accurately lay claim to the title. Physicians apparently recognize this as well, as they have consistently begun to use the term “physician anesthesiologist.” It is not uncommon for surgeons and patients to refer to the CRNA as an “anesthesiologist” while being fully cognizant of their nursing education. Therefore, use of “nurse anesthesiologist” to describe CRNAs would not be confusing. Rather, the term would be clarifying and likely remove confusion regarding the role of the CRNA as a fully qualified and often independent provider of anesthesia.
Language and etymology
Both “anesthetist” (one who administers anesthesia) and “anesthesiologist” (one who has studied the science of anesthesia) are accurate titles for expert CRNAs and physicians specializing in anesthesia. While dictionaries may refer to a physician performing anesthesia as an “anesthesiologist,” dictionaries can be updated, whereas the etymology of words remains intact despite updated definitions.
Counterarguments
No title can be used if the title is not legally authorized
The argument could be advanced that a CRNA should not use the term because no law specifically permits a title other than CRNA. This argument stems from the notion that the legislature, in providing a title for CRNAs to use, declared that no other title or term could be used. The use of CRNA as a protected title is discussed below.
If the law does not expressly limit the title that can be used, it would be a stretch to conclude that the law should be construed to mean that the reserved title is the only title that can be used. Clearly, it might be argued that the legislature intended a CRNA to be permitted to use only the specifically created title. However, if the law addresses who may use the specific title, that reservation should not be given a broader construction that the title limits both who may use the title and limits what title the user must use or may only use. Indeed, many examples exist throughout the medical professions allowing the use of other descriptors or titles that are recognized by associations, facilities, and individuals such as Advanced Practice Provider, mid-level provider, Advanced Practice Registered Nurse, and Anesthesia Provider.
In short, if the law does not declare that a CRNA may use only a specific title, the argument that the law restricts the use of a title only if legally authorized would be incorrect.
A protected title already exists for CRNAs
A separate but related objection might be raised that CRNAs already have a reserved title, and therefore the CRNA should not also be permitted to use another title or descriptor. This argument rests on the foundation that the legislature’s creation of a title and reservation of the use of this title by only those who had been educated, met qualifications and demonstrated competence, meant to do more than prevent the public from being misled by those who hold themselves out as CRNAs. When the legislature directed that only those who are qualified may apply for and use the designated credential, the legislature had a purpose of preventing the public from being misled by others lacking the education and training, who might use the title to create the impression of a competency and practice scope that had not been conferred by law.
As noted previously, if the law does not restrict the use of any other title, it would be a stretch to reach the conclusion that the law must be understood and applied to prohibit the use of any title other than the reserved title.
Again, the argument could be advanced that with a title created by statute, as a matter of judgment, those given exclusive use of title should use that title, and by failing to use that title, the grant created by the law is being undervalued or squandered. But the application of a law to restrict others from using a title to declare that those who may use that title may only use that title, would be a misreading of the law absent an express declaration in the law to this effect. Clearly, to make this argument, it would have to be argued that the legislature had intended a CRNA to be permitted to use only the specifically created title.
However, against a backdrop in which the law does not expressly contain this limitation, the better argument would seem to be that the law does not have this meaning or effect.
In short, if the law does not declare that a CRNA may use only a specific title, the argument that because the law gives CRNAs the exclusive use of a title, it would be incorrect that this is the only title that may be used.
The use of “nurse anesthesiologist” could be misleading
The argument could be made that the use of the term “nurse anesthesiologist” is misleading. However, if this argument is advanced, the argument must be more fully understood and analyzed to determine in what way the title or term is misleading.
First, does the use of the title convey the impression that the nurse is being passed off as a physician? Given the ASA’s own research, it would follow that the use of the title cannot – and should not – be understood to convey the meaning that the user is a physician because the title makes clear that the user is a nurse.
Second, does the use of the title convey the impression that the nurse is being passed off as a person able to provide services that include anesthesiology when the law does not permit these services to be provided by that person? Assuming the scope of practice that the person is legally permitted to perform includes the performance of services that include anesthesiology by law then it would follow that the use of the title cannot – and should not – be understood to convey a misleading meaning. Assuming CRNAs are allowed by law to provide services that include anesthesiology, then it follows that the use of the title is not misleading on this ground.
Anesthesiologist is already defined as a physician in certain states
“Anesthesiologist” has a statutory definition in 3 states. While legal opinions will undoubtedly vary whether “nurse anesthesiologist” and “anesthesiologist” are legally distinct terms, it remains that adding the title “nurse” must influence the meaning of the word that follows even in the most conservative interpretation. It is notable that other states (18) have regulatory definitions of “anesthesiologist”. However, these laws must be interpreted in light of the fact that the ASA now refers to its members as “physician anesthesiologists” (see end packet insert). None the less, members should use detailed consideration and judgement as to the specifics of the law in their state.
Additionally, precedent demonstrates that the AANA advocates on behalf of its members on most issues using a state-by-state approach (i.e., pain management) and the term remains completely optional for members to use based upon state law and prudent discretion.
The use Nurse Anesthesiologist could trigger lawsuits
No law prohibits the use of this identifier. The possibility that others might mount a campaign – or a lawsuit – to challenge the use of the title is just that – a possibility. But this possibility does not mean such an effort is correct or will succeed. Instead, the question to be resolved should focus on whether the legal (including policy) arguments that might be advanced would gain acceptance. And the resolution of this question would necessitate an analysis of the basis of the legal arguments.
As outlined above, with the assumption that the law does not bar the use of “nurse anesthesiologist,” and having discussed whether the law can be construed not to limit the title that CRNAs may use and that the use of the term is not misleading, another question might be whether the use of the title is somehow reserved as a matter of intellectual property law. Although beyond the scope of this discussion, recent efforts to achieve intellectual property protection for the title “nurse anesthesiologist” have failed because the title is viewed as too generic. If this is true for nurses, the conclusion would seem to be equally true for medical doctors.
Nurse Anesthesiologist is not protected
One additional argument against the use of the title or term “nurse anesthesiologist” could be that it is not protected. In other words, because the title is not protected, it may not be used.
A variation of this argument has already been explored in an earlier discussion about whether the law restricts the title that CRNAs may use. As with that argument, the conclusion that absence of title protection infers that the title cannot be used would seem to be an overstatement. Otherwise, a similar argument might be made that no one may use the title “anesthesiologist” because no protection exists for the use of this title by any person and no law restricts the use of this title by members of a given profession. But it would be absurd to make the argument that because no title protection exists in the medical field, the law bars a physician who practices and is qualified and trained to provide anesthesiology services from being held out to the public as an anesthesiologist. This same conclusion should be sufficient to address this final objection.
“In every jurisdiction in which CRNAs practice, the scope of physicians and CRNAs involves the delivery of anesthesia, i.e., the practice of anesthesiology. As such rather than trying to endlessly compare or fight, participants in this dialogue should be motivated to recognize that both CRNAs and physicians, as experts in the field, work together to maximize benefit for patients and society. ”
In every jurisdiction in which CRNAs practice, the scope of physicians and CRNAs involves the delivery of anesthesia, i.e., the practice of anesthesiology. As such rather than trying to endlessly compare or fight, participants in this dialogue should be motivated to recognize that both CRNAs and physicians, as experts in the field, work together to maximize benefit for patients and society. Despite the ASA’s insistence that nurse anesthetists are equivalent with their assistants, “Nurse Anesthesiologist” is not meant as a provocation, but instead as a point of clarity that multiple professionals are experts in the field of anesthesia. If the ASA has issue with the undeniable fact that nurse anesthetists are, in fact, experts – then we can only suggest they realize that working together we can generate more benefit for patients than by trying to minimize one another.